What Are Allergies?
Antibodies have an important role in our body. When we are ill our antibodies recognize foreign invaders so that our body can neutralize them and respond appropriately. This is critically important bodily process but extremely inconvenient when this same process occurs to inert environmental proteins, the type of proteins our immune system should recognize as benign. This article will address specifically seasonal and environmental allergies including:
- Cat dander allergy
- Dog dander allergy
- Dust mite allergy
- Tree pollen allergy
- Grass allergy
- Weed allergy
- Mold allergy
What Are Allergy Symptoms?
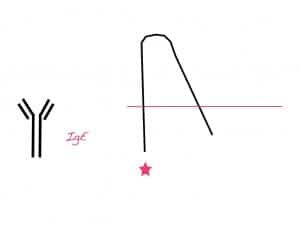
When IgE antibodies react to protein it causes a histamine response. The release of histamine results in typical allergy symptoms such as runny nose (hayfever, allergy rhinitis) and itchy eyes.
Treatment For Allergies
The most common allergy strategies focus on upstream management of allergic symptoms. Upstream management means treating the symptoms of allergies.
The most common way to address environmental and seasonal allergies are through the use of anti-histamines. Anti-histamines medications are indeed quite effective at reducing and eliminating allergic symptoms. There are also some natural supplements that help minimize histamine release by stabilizing the mast cells that secrete histamine. I call this upstream management because it is a quick fix to address the symptoms as a result of the histamine release. The reality is however it is only addressing one of the last steps in the chain of command. This means long standing dependence on this type of treatment is needed. Whether you choose antihistamine medication or specific natural antihistamine and mast cell stabilizers the action occurs late in the game and is not addressing the immune dysfunction.
A Paradigm Shift: Downstream Management
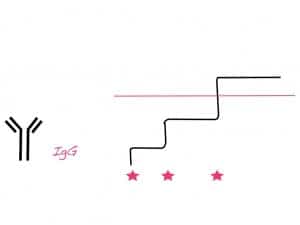
Sublingual immunotherapy treats the underlying immune dysfuntion. This is what I call downstream management because when you address the initial aberrant reaction you eliminate the following chain of command that leads to histamine release in the first place.
Sublingual immunotherapy (SLIT) is a proven therapy that is often overlooked as an option for allergy treatments. There are over 60 clinical trials proving efficacy for allergic rhinitis (runny nose) and allergic conjunctivitis (itchy eyes). It has also been found to prevent the development of allergic asthma in children with eczema (atopic dermatitis) and allergic rhinitis (runny nose). It’s a therapy that is endorsed by the World Health Organization, the World Allergy Organization and the Cochrane Collaboration.
A Paradigm Shift In Allergy Treatment
If you are serious about taking charge of you allergies permanently then start treating the problem downstream at the source. Retraining your immune system using SLIT does involve commitment. It is not a process that occurs overnight but it is a treatment for allergies that can be permanent if done as prescribed. Check out more information about Sublingual Immunotherapy here.